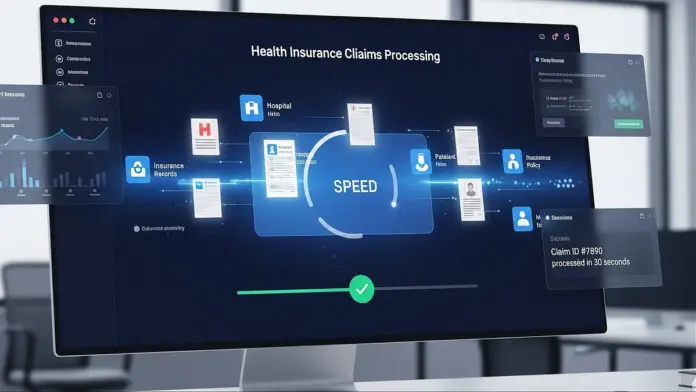
Reimbursement claims can be a tedious process, requiring employees to gather documents, send emails, and follow up with Third-Party Administrators (TPAs), often leaving them in uncertainty. Unlike cashless claims, where hospitals and insurers directly handle payments, reimbursement claims demand significant effort from employees. ClaimSetu streamlines this experience, simplifying each step of the reimbursement journey. By leveraging user-friendly tools and efficient tracking systems, ClaimSetu minimizes confusion and enhances transparency, making the reimbursement process smoother and faster. With ClaimSetu’s innovative approach, employees can navigate the complexities of reimbursement claims with ease, ensuring timely submissions and better communication with TPAs. This not only saves time but also reduces frustration, empowering users to focus on what truly matters—recovering quickly without the hassle of unresolved claims. Ultimately, ClaimSetu transforms the reimbursement claims experience into a more manageable and efficient process, contributing to greater employee satisfaction.
Source link
Discover ‘ClaimSetu’: India’s Pioneering AI Solution for Accelerating Group Health Insurance Reimbursement Claims
Share
Read more